Understanding the epidemiology and perceived efficacy of cannabis use in patients with chronic musculoskeletal pain
Leroux, T., Ajrawat, P., Sundararajan, K. et al. Understanding the epidemiology and perceived efficacy of cannabis use in patients with chronic musculoskeletal pain. J Cannabis Res 6, 28 (2024). https://doi.org/10.1186/s42238-024-00231-1
Abstract
Background
The belief that cannabis has analgesic and anti-inflammatory properties continues to attract patients with chronic musculoskeletal (MSK) pain towards its use. However, the role that cannabis will play in the management of chronic MSK pain remains to be determined. This study examined 1) the rate, patterns of use, and self-reported efficacy of cannabis use among patients with chronic MSK pain and 2) the interest and potential barriers to cannabis use among patients with chronic MSK pain not currently using cannabis.
Methods
Self-reported cannabis use and perceived efficacy were prospectively collected from chronic MSK pain patients presenting to the Orthopaedic Clinic at the University Health Network, Toronto, Canada. The primary dependent variable was current or past use of cannabis to manage chronic MSK pain; bivariate and multivariable logistic regression were used to identify patient characteristics independently associated with this outcome. Secondary outcomes were summarized descriptively, including self-perceived efficacy among cannabis users, and interest as well as barriers to cannabis use among cannabis non-users.
Results
The sample included 629 patients presenting with chronic MSK pain (mean age: 56±15.7 years; 56% female). Overall, 144 (23%) reported past or present cannabis use to manage their MSK pain, with 63.7% perceiving cannabis as very or somewhat effective and 26.6% considering it as slightly effective. The strongest predictor of cannabis use in this study population was a history of recreational cannabis use (OR 12.7, p<0.001). Among cannabis non-users (N=489), 65% expressed interest in using cannabis to manage their chronic MSK pain, but common barriers to use included lack of knowledge regarding access, use and evidence, and stigma.
Conclusions
One in five patients presenting to an orthopaedic surgeon with chronic MSK pain are using or have used cannabis with the specific intent to manage their pain, and most report it to be effective. Among non-users, two-thirds reported an interest in using cannabis to manage their MSK pain, but common barriers to use existed. Future double-blind placebo-controlled trials are required to understand if this reported efficacy is accurate, and what role, if any, cannabis may play in the management of chronic MSK pain.
Introduction
Musculoskeletal (MSK) disorders are the most common cause of functional disability and chronic pain worldwide (Pinto et al. 2017; Sundstrup et al. 2016). Osteoarthritis (OA) is a common cause of MSK related pain and disability with persistent pain typically being the catalyst for seeking medical intervention (Pinto et al. 2017; Yelin et al. 2016). As the global population ages, the burden of chronic MSK pain is expected to rise, substantially increasing societal costs and healthcare resource utilization (Pinto et al. 2017; Yelin et al. 2016). Current pharmacological (NSAIDs, COX-2 inhibitors, acetaminophen, serotonin-norepinephrine reuptake inhibitors, anticonvulsants, opioids, gabapentinoids) and non-pharmacological (physiotherapy, acupuncture, mindfulness/psychotherapy, transcutaneous electrical nerve stimulation therapy, etc.) approaches to manage chronic MSK pain have at best delivered modest efficacy and can often cause harmful adverse events. Given the unreliability of these therapies, it is not surprising that many chronic MSK patients often seek non-opioid and non-surgical alternatives for pain management (Boehnke et al. 2019).
Recreational cannabis use is now legal in several countries and there is a trend towards further legalization globally. More recently, the use of cannabis as an analgesic, immunomodulatory, and anti-inflammatory agent for patients with chronic MSK pain has become relevant (Ajrawat et al. 2022; Meng et al. 2021). Studies have shown the endocannabinoid system to be expressed in various cell types within human joints, including synovial cells, chondrocytes, and bone cells (Dunn et al. 2016; Porta et al. 2014). Clinical cannabinoid research to date has largely focused on neuropathic pain or chronic non-cancer pain (CNCP), with previous studies indicating that 10-15% of chronic pain patients use cannabis to manage their pain (Piper et al. 2017; Haroutounian et al. 2016; Hazekamp et al. 2013; Troutt and DiDonato 2015). Prior systematic reviews have demonstrated cannabis’ effectiveness in managing chronic pain and potentially reducing opioid consumption (Troutt and DiDonato 2015; Whiting et al. 2015). A study observing 757 patients who used a combination of dried or oil-based cannabis formulations revealed that, after 12 months of follow-up, the percentage of individuals reporting opioid use decreased by approximately half, dropping from 40.8% to 23.9% (Meng et al. 2021). Another study investigated chronic osteoarthritis (OA) patients, most of whom were using either cannabidiol (CBD) or tetrahydrocannabinol (THC) products in a sublingual tincture form. The findings revealed lower pain scores, improved quality of life, and a decrease in morphine milligram equivalents (MME) among these patients with 37.5% of participants achieving 0 MME/day at the 6-month follow-up (Renslo et al. 2022). A third cross-sectional study investigated the use CBD on arthritic symptoms among OA, rheumatoid, and other autoimmune arthritis patients. The authors reported that while all groups lowered their medications use and improved their arthritic symptoms, the OA group had the greatest improvements in physical function and pain with CBD use (Frane et al. 2022). Although past studies have been promising, these effects are still poorly investigated in patients experiencing chronic MSK pain, limiting the generalizability to this large patient population.
Therefore, the purpose of the present study was 1) to determine the patient reported prevalence rate, patterns of use, and perceived efficacy of cannabis use among patients with chronic MSK pain (i.e., pain on most days for at least three months duration) referred for orthopaedic consultation and 2) to identify the interest and potential barriers to cannabis use among patients with chronic MSK pain not currently using cannabis.
Methods
Study design and setting
In this cross-sectional study, we administered an anonymous electronic survey regarding cannabis use to consecutive patients presenting with chronic MSK pain to the Orthopaedic clinic at the University Health Network (UHN), Toronto, Canada. All potentially eligible patients visiting the clinic between November 1, 2018 and April 30, 2019 were informed of the study by a designated member of the patient’s circle of care. If the patient expressed interest, a research assistant obtained electronic written consent via a tablet and confirmed the patient’s eligibility, then invited the patient to complete the tablet-based survey (Supplementary Tables 1-3). The study was approved by the UHN Research Ethics Board (REB Number: 18-5716).
Participants
Patients with chronic MSK pain who were visiting the Orthopaedic Clinic at Toronto Western Hospital, University Health Network for a first-time consultation with an orthopaedic surgeon were included. Patients were deemed eligible to participate if they met the following inclusion criteria: (1) were ≥18 years of age, (2) able to speak and comprehend English, (3) and reported having chronic MSK pain, defined as muscle, tendon, bone or joint pain on most days for at least three months duration. Patients were excluded if they had sustained an acute MSK soft-tissue injury or fracture in the past 6 months, or if they had undergone surgery in the past 6 months.
Development of survey
The survey was designed to collect data on patient demographics, current health status and pharmaceutical pain management, characteristics of MSK pain, and cannabis use. A team of surgeons and clinical experts in the field self-developed the survey. To create it, we utilized questions from the Longitudinal Evaluation in the Arthritis Program (LEAP) study as a foundation and then developed questions specific to cannabis use based on the available literature (Whiting et al. 2015; Walsh et al. 2013; Power et al. 2019). Although this survey was not internally or externally validated, 3-4 research personnel reviewed the questionnaire on iPads to ensure clarity, coherence, and technical functionality before administering it to patients.
All respondents completed the demographics, health status, and cannabis use sections of the survey (Supplementary Table 1). Respondents who reported current or past use of cannabis to manage MSK pain (“cannabis users”) also answered more detailed questions regarding their duration and frequency of cannabis use, strain/type consumed, monthly cost, mode of administration, provenance, cannabis-related side-effects, and reason for initiating use (Supplementary Table 2). Cannabis users were also asked to report their perception of cannabis’s effectiveness for alleviating chronic MSK pain, its effectiveness compared to other prescription medication(s) and change in use of other medications since starting to use cannabis. Respondents who reported never using cannabis to manage MSK pain (“cannabis non-users”) were asked to rate their interest in using cannabis to manage chronic MSK pain, as well as potential barriers to using cannabis for this purpose (Supplementary Table 3).
Outcomes
The primary outcome of this study was current or past cannabis use for chronic MSK pain management, defined as a response of “yes” on the question “Have you ever used cannabis to manage your musculoskeletal pain (which includes muscle, tendon, bone or joint pain)?” Secondary outcomes were stratified based on reported cannabis use for the purposes of managing chronic MSK pain. Among cannabis users, secondary outcomes included patterns of cannabis use, self-perceived effectiveness, and self-reported changes in pain medications with cannabis use. Among cannabis non-users, secondary outcomes included interest in using cannabis for the management of chronic MSK pain and barriers to its use.
Covariates
Patient demographics (age, gender, ethnic group, education, labour force participation, household income, and body-mass index), comorbid conditions, use of other pain medications (over-the-counter analgesics, prescription non-steroidal anti-inflammatory drugs, muscle relaxants, narcotic drugs, antidepressant drugs, and neuroleptic drugs), pain characteristics (bodily region for which the respondent is seeking care, number of painful bodily regions, and duration of pain), history of chronic pain specialist consultation, and recreational cannabis use were assessed as potential predictors of cannabis use for the management of chronic MSK pain.
Data extraction and collection
Participants entered survey responses directly into an electronic database via a tablet-based survey application. Analyses were carried out in R Statistical Software version 3.6.1 (Rdct and R: A, 2011).
Statistical analysis
Patient characteristics, patterns of cannabis use, and its self-perceived effectiveness and side effects were summarized descriptively; continuous measures were summarized with means and standard deviations, and categorical measures with counts and percentages. Bivariate analysis was conducted comparing cannabis users (patients reporting current or past cannabis use to manage their chronic MSK pain) versus non-users (patients who reported never using cannabis to manage MSK pain), using the Mann-Whitney test for continuous variables and Fisher’s exact test for categorical variables. We expected that approximately 5% of patients who visit the orthopaedic clinic will use cannabis, based on data from Ste-Marie and colleagues (Liu et al. 2019). The minimum sample size is given by n = (z/m)^2 x p(1-p), where Z is the z-score corresponding to the desired confidence level, m is the desired level of precision, and p is the expected proportion of patients who use cannabis for therapeutic purposes. With Z = 1.96, m = 0.05, and p = 0.05, the minimum required sample size is 73 participants.
P-values from bivariate analysis were adjusted to control false discovery rate (FDR) (Benjamini and Hochberg 1995). To identify factors independently associated with medical cannabis use, factors found to be significantly associated with cannabis use in the bivariate analysis (p < 0.05) were entered in a multivariable logistic regression model of cannabis use along with age, gender, and ethnicity. Model fit was assessed with the area under the receiver operator curve and McFadden’s pseudo-R2. Results of the multivariable logistic regression were reported as Odds Ratios (OR) with 95% confidence intervals (CI). After reviewing bivariate analysis results, the following terms were entered into the model: age; gender; ethnicity (coded as White vs. non-White); labour force participation (coded as working/looking for work/short-term disability, retired/homemaker/student/other, or not looking for work/long-term disability); self-reported depression; number of comorbid conditions reported, excluding depression and MSK pain conditions (coded as none, 1-2 conditions, or 3+ conditions); use of narcotic medication (coded as never vs. sometimes/daily); ever visiting a pain clinic or specialist; bodily region for which the respondent is seeking treatment (coded as upper extremity, lower extremity, or spine); total number of painful bodily areas (coded as 1, 2, 3, or 4+ areas), duration of MSK pain (coded as 0-1 years, 1-5 years, or 5-10 years), and history of recreational cannabis use (coded as never vs. current/former use).
Results
Patient characteristics
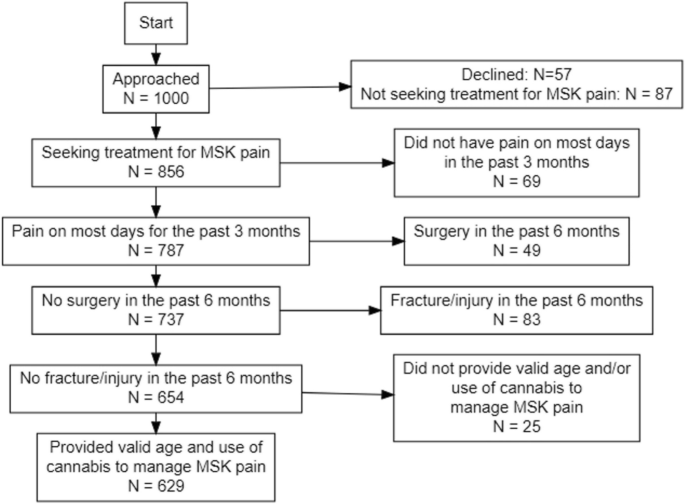
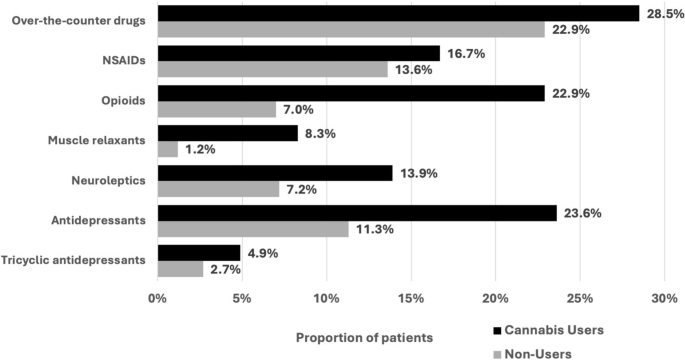
One thousand patients presented to the orthopaedic clinic and were approached for study enrolment, of which 629 met the inclusion criteria and were included (Fig. 1). A total of 144 (23%) patients reported any (previous or current) cannabis use with the specific intention of managing their chronic MSK pain, of which 72% (N=104) were currently using cannabis to manage their pain. Cannabis users had a mean age of 50.88 ± 15.31 years and 51% (N=73) were females (Table 1). In comparison to cannabis non-users, cannabis users reported higher use of daily pain medications (Fig. 2).
In the bivariate analysis comparing cannabis users to non-users (Tables 1 and 2), cannabis use was associated with younger age (p < 0.001) and employment status (p=0.002), with users more likely to report being unemployed or on long-term disability. Cannabis users were more likely to have multiple comorbid conditions (p = 0.002), including depression (p < 0.001), back pain (p < 0.001), chronic neck pain (p < 0.001), and chronic pelvic pain (p < 0.001). They also reported a larger number of painful bodily areas (p < 0.001), longer pain durations (p = 0.003), more often visited a pain clinic/specialist (p = 0.003), and more frequently used muscle relaxants (p = 0.002), opioids (p = 0.002), and antidepressants (p = 0.002). Cannabis users were also more likely to report recreational cannabis use (p = 0.001). There were no statistically significant differences between cannabis users and non-users in sex, ethnicity, educational attainment, or income.
Patterns of cannabis use
A descriptive summary of cannabis users’ survey responses is presented in Table 3. Twenty-seven percent reported using cannabis for two or more years, and 25% for less than six weeks. Most patients used cannabis daily (59%). Thirty-nine percent of cannabis users reported spending at least $100 per month on cannabis products (Table 3).
Among cannabis users, CBD was the most commonly used cannabinoid (39%), followed by 20% of users consuming a hybrid of various cannabinoids. Twenty-three percent of cannabis users were unaware of their cannabis composition. The most frequent modes of administration among cannabis users were the ingestion of oils (57%), smoking (36%), and vaporizing (32%).
Twenty-six percent of users reported that they started using cannabis for pain management on the recommendation of a physician, and an equal proportion reported that a friend or relative advised them to use cannabis to manage pain (the options were not mutually exclusive). Many users reported getting cannabis from more than one source, including a dispensary or compassion club (43% of users); a Health Canada licensed provider (34%), and from a friend or relative (33%, Table 3).
Perceived effectiveness
The majority of cannabis users noted effective pain management from cannabis, with 63.7% describing it as very or somewhat effective and 26.6% indicating it as slightly effective (Table 3). Fifty-seven percent of users indicated cannabis to be more effective than other analgesic medications at managing their chronic MSK pain (Table 3). Forty percent of users reported that their use of other analgesic medication had decreased since starting to use cannabis, while 58% of cannabis users indicated no change in their analgesic medication usage since initiating cannabis (Table 3).
Commonly reported cannabis-related side effects included dry mouth (43%), fatigue (23%), and a lack of motivation (15%). Thirty-nine percent of cannabis users experienced no cannabis-related side-effects. Many users indicated cannabis’s effectiveness in treating other symptoms, primarily sleep disturbances (44%), anxiety (26%), and headaches (18%). Forty-three percent of cannabis users experienced no other symptomatic reliefs.
Predictors of current or past use of cannabis for MSK pain
Results of the multivariable regression analysis are illustrated in Table 4. The most significant predictor of cannabis use was current or previous recreational cannabis usage (OR:12.72, p = < 0.001). Other significant independent predictors of cannabis use included self-reported depression (2.17, p = 0.01); opioid medication use (1.78, p = 0.03); history of pain clinic/specialist visits (1.93, p = 0.01); seeking treatment for spine pain versus lower extremity pain (2.14, p = 0.01); a greater number of painful bodily areas (2.28 for three [p = 0.04] and 2.57 for four or more areas [p = 0.01], versus one area); and increased duration of MSK pain (2.28 for one to five years [p = 0.04] and 2.8 for five to ten years [p = 0.01], versus less than one year). While controlling for these factors, age, gender, ethnicity, labour force participation and number of comorbid conditions were not significant predictors of cannabis use for MSK pain management.
Non-cannabis users
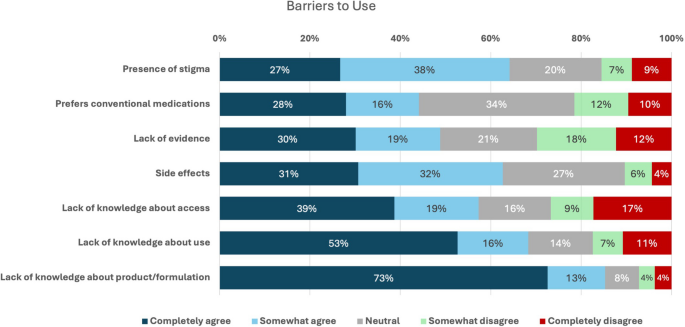
Sixty-five percent of cannabis non-users reported an interest in using cannabis for managing their chronic MSK pain. Given a list of potential barriers to using cannabis, the majority of non-users “completely” or “somewhat” agreed with many of the barriers, especially a lack of knowledge regarding cannabis formulations (85%), how to use cannabis for pain management (68%), and how to access cannabis for pain management (57%,); potential cannabis-related side effects (63%); and a perception of stigma (64%) (Fig. 3).
Discussion
In this study, more than one in five patients presenting to an orthopaedic surgeon with chronic MSK pain had used or was currently using cannabis to manage their chronic MSK pain. Consistent with previous self-reported studies, the majority of these patients perceived cannabis to provide effective pain management (Ajrawat et al. 2022; Meng et al. 2021). More than half (57%) claimed cannabis to be more effective than other analgesic medications, and 40% reported decreasing their use of other analgesic medications since starting cannabis use. Only 26% of cannabis users reported that a physician recommended the use of cannabis to manage their chronic MSK pain, and 23% were unaware of the composition of the cannabis they were consuming. Among non-users, 65% expressed an interest in using cannabis for managing their chronic MSK pain but often reported that they lacked knowledge regarding efficacy, access, usage, and composition, as well as the associated stigma.
We found that 23% of chronic MSK pain patients have used or are using cannabis to manage their pain, of which the majority are current users (72%). This rate of cannabis use among chronic MSK pain patients in the present study is considerably higher than the cannabis use rates reported in past studies with similar patient populations. For instance, two different studies, one from Canada and another from the United States, indicated that 4% of patients undergoing orthopaedic procedures used cannabis (Liu et al. 2019; Medina et al. 2019). Similarly, a 2014 Canadian study reported that approximately 3% of rheumatology patients were cannabis users (Ste-Marie et al. 2016). Yet, a more recent study conducted in Canada revealed that 29% of individuals with upper extremity conditions were presently utilizing cannabis, primarily for the purpose of pain management (Greis et al. 2022). The difference in prevalence between the previous studies from 3-6 years ago and the current study is largely due to the legalization of cannabis in Canada in October 2018, resulting in potential changes in attitudes towards and acknowledgment of use and more permissive access to cannabis without stigma and/or legal implications. In fact, a study assessing data from the National Cannabis Survey (NCS) revealed that in the months preceding legalization, 19% of Canadian respondents intended to try cannabis or increase their cannabis use following legalization (Sandhu et al. 2019). Complementing this, a 2014 US survey found that 13.5% of people would consume cannabis more frequently if legalized (Cohn et al. 2017). Additionally, the anonymous self-reported nature of the current study may have also allowed patients to feel comfortable disclosing their cannabis, resulting in the higher rate we observed.
The strongest predictors of those who would use cannabis for managing their chronic MSK pain, were patients with a history of recreational cannabis use and the presence of long-term chronic pain. These findings are consistent with previous reports examining cannabis use in various patient populations (Liu et al. 2019; Medina et al. 2019; Sandhu et al. 2019; Bhashyam et al. 2019). It was found that previous recreational cannabis use was associated with a more than tenfold increase in the odds of using cannabis to manage chronic MSK pain. This was unsurprising as current cannabis use has been shown to strongly influence one’s perceptions of risk, stigma, and acceptability (Rudski 2014). Features consistent with the diagnosis of a chronic pain syndrome, such as frequent pain clinic visits and longer pain duration, were also strong predictors of cannabis use in the current cohort, suggesting that patients with chronic MSK pain are possibly unsatisfied with conventional treatments and seeking alternative pain therapies. Lastly, younger age was not a predictor of using cannabis for the management of chronic MSK pain, when controlling for factors such as opioid consumption, depression status, and the duration of pain. This finding is inconsistent with past studies which have indicated that the incidence of any cannabis use (medical or recreational) generally declines with increasing age (Rotermann and Page 2018; Sampasa-Kanyinga et al. 2018). Typically, it is assumed that younger age is associated with cannabis use, which is likely because the belief among younger adults is that cannabis use is socially acceptable, not addictive, and not harmful (Kandel 2002; Keyhani et al. 2018; Ware et al. 2003). However, there may be several potential reasons for this discrepancy. First, the current study’s cohort is older overall (mean age >50 years) and includes fewer young adults that would typically report a greater prevalence of use as compared to elderly patients. Second, this finding may suggest a growing acceptance among older patients regarding the role of cannabis use for the purpose of managing medical issues, which may be the result of the legalization in Canada, increasing societal acceptance, and improvements in accessibility of non-inhaled cannabis products.
In this study, over 85% of cannabis users perceived it to be effective in managing their chronic MSK pain and improving their sleep and anxiety-related symptoms. Several studies have also noted similar rates of perceived effectiveness in chronic pain patients (Heng et al. 2018; Miller and Miller 2017; Mucke et al. 2018). One study with 937 orthopaedic outpatients found that cannabis use was significantly associated with decreased pain intensity and better lower extremity activity scores (Medina et al. 2019). In a prospective observational study of chronic orthopaedic pain patients, medical cannabis use was associated with significant clinical improvements in VAS pain scores, global physical health and mental health, and quality of life within three months but plateaued at the 6 and 12 month follow-up periods (Greis et al. 2022). Furthermore, cannabinoids were found effective in all eight studies from a systematic review that evaluated chronic pain stemming from orthopedic etiologies (Vivace et al. 2021). Despite preliminary evidence suggesting cannabis’ pain management potential, most studies have short-term follow-ups with relatively small sample sizes. Moreover, significant heterogeneity exists among studies with regards to dosage, routes of administration, composition, frequencies, and patient populations, justifying the need for further investigations to elucidate the true efficacy of cannabis for the management of chronic MSK pain.
Several interesting observations were noted herein: a quarter of cannabis users had no knowledge of the current cannabis product they were consuming and only a third of users procured their cannabis from a Health Canada licensed provider. A study with upper extremity orthopaedic patients indicated that approximately 46% of patients felt more comfortable discussing their cannabis use with their physician after legalization (Sims et al. 2022). From a recent survey study, 86% of orthopaedic patients that were characterized as cannabis users stated that they would be willing to stop consuming cannabis if their surgeon stated it would adversely impact their surgery (Carney et al. 2020). These observations highlight the dire need for improved oversight and regulation of the medicinal cannabis industry (Craft et al. 2020; Freeman and Lorenzetti 2020). In the present study, 23% of cannabis users were unaware of their cannabis composition. Greis and colleagues reported similar findings with 23-29% of orthopaedic patients being able to estimate the cannabis composition of their inhaled or oral cannabis products (Greis et al. 2022). In our study, the most frequent modes of administration among cannabis users were the ingestion of oils (57%), smoking (36%), and vaporizing (32%). Similar to our results, a previous report indicated that most orthopaedic patients preferred oral or sublingual administration of cannabis followed by inhalation to manage their chronic pain (Greis et al. 2022). In contrast, Carney et al reported that smoking was the most common mode of administration, followed by edible products, and vaporizing (Carney et al. 2020). Although most patients in the present study reported cannabis to be effective, the varying compositions, dosages, frequencies, and routes of administration, suggests that placebo may mitigate some of the perceived efficacy. As such, there is a need for large scale observational studies where the dosages and route of administration are standardized. This could then lead to meaningful placebo-controlled comparative studies in similar patient populations to determine the effectiveness on symptom management.
Historically, common first-line pharmacologic treatments such as nonsteroidal anti-inflammatory drugs (NSAIDs) have been prescribed to alleviate chronic pain. However, NSAIDs have been associated with intolerance and serious adverse events in some patients including upper gastrointestinal bleeding or perforation (Bjordal et al. 2004; Langman et al. 1994). Opioids have also been prescribed to manage chronic MSK pain when conventional treatments have failed, so it is not surprising that individuals with chronic MSK pain are amongst the highest prescription opioid users (Ashaye et al. 2018; Manchikanti et al. 2012). However, long-term opioid use has been associated with greater pain intensity, poorer outcomes, and unintendedly increases the risk of developing an opioid use disorder, diversion, and fatal overdose (Bot et al. 2014; Dunn et al. 2010; Koehler et al. 2018; Noble et al. 2010). Cannabis has been suggested as a potentially safer analgesic therapy. In the present study, approximately 40% of our patients reported that their analgesic medications were reduced after initiating cannabis. A similarly designed study by Sims and colleagues with reported that 51% of orthopaedic patients felt that cannabis was safer than their prescription analgesics. (Sims et al. 2022) Further, Greis et al reported that 31% of chronic orthopaedic pain patients discontinued benzodiazepines, 73% either ceased or decreased opioid consumption, and noted a 23.4% reduction in 6-month total opioid prescription with cannabis use (Greis et al. 2022). Moreover, a systematic review evaluating the use of cannabinoids in orthopaedic patients found that the five of the seven studies noted an opioid sparring effect and two of the seven studies reported complete cessation of opioid use at the 6 to 12 month follow-up period (Vivace et al. 2021). Prior surveys of American and Canadian cannabis users reported that substituting cannabis for opioids resulted in improved pain management, decreased adverse effects, and eased opioid withdrawal symptoms. (Lucas and Walsh 2017; Vyas et al. 2018)
It is noteworthy that cannabis users exhibited a constellation of comorbid conditions, including a higher prevalence of depression and pain, an increased number of painful bodily areas, longer pain durations, and more frequent visits to pain clinics/specialists when compared to non-cannabis users. This observation prompts us to consider the possibility that cannabis use may have arisen as a response to elevated levels of pain and dissatisfaction with existing therapeutic modalities. It is possible that a significant proportion of cannabis users turned to cannabis to seek relief from their heightened pain burden, which appears refractory to conventional treatments. Furthermore, we observed that cannabis users, despite experiencing greater pain, tended to employ a broader array of medications, such as muscle relaxants, opioids, and antidepressants, in comparison to their non-cannabis-using counterparts. This may also highlight that cannabis may have been sought as an alternative means of pain management, especially in situations where previous therapies yielded suboptimal results.
In this cohort, approximately two-thirds of cannabis non-users expressed interest in using cannabis for managing their chronic MSK pain, but often reported that they lacked knowledge regarding efficacy, access, usage, and composition. Interestingly, stigma was not a primary concern for cannabis non-users as previously cited in the literature (Bottorff et al. 2013; Hathaway et al. 2011; Satterlund et al. 2015), possibly attributed to the recent cultural shifts with cannabis legalization and with the increasing number of cannabis products that do not need to be smoked for consumption (only one third of products consumed in this study were smoked), leading to greater social acceptability and normalization (Hathaway et al. 2011). Research indicates that individuals are learning about cannabis from acquaintances and the internet instead of healthcare professionals (Corroon and Phillips 2018), which is consistent with the findings of the current study whereby only a quarter of patients started using cannabis as a result of a physician’s recommendation. Although the general perception is that cannabis is safe, there is a potential for side effects and drug interactions of which patients need to be aware (Alsherbiny and Li 2018; Iffland and Grotenhermen 2017). However, a lack of confidence regarding their knowledge on cannabis safety and efficacy exists among physicians (Fitzcharles et al. 2014; Kondrad and Reid 2013), which may prevent them from either initiating or participating in discussions regarding medical cannabis use with their patients. As such, continuing education initiatives targeting physicians are important to ensure they are armed with basic, albeit necessary, information regarding medical cannabis.
With the increased legalization of cannabis across North America and the clear interest by MSK pain patients to use cannabis therapeutically, there is large knowledge gap to fill in understanding the role of cannabis, if any, in managing chronic MSK pain. Future investigations should aim to conduct high-quality multicentre double-blind placebo-controlled trials with larger sample sizes and longer durations to assess the clinical efficacy and the long-term adverse events of cannabis as a monotherapy and in conjunction with standard analgesics. Future studies should aim to determine the optimal dosage, dose-response effects, drug interactions, and the ideal composition and route of administration based on patient history and preference.
Limitations
This study has several limitations. First, the survey utilized was not validated and the inability to compare characteristics of study participants with non-participants (i.e., those who declined or weren't eligible) limits the capacity to assess the external validity of the research. Second, the prevalence of cannabis use may be understated, given the stigma often associated with cannabis use and the use of self-reported data. However, the anonymous nature of the survey may have minimized this concern. Third, recall bias may have occurred with cannabis-related information, possibly affecting data accuracy. Additionally, the higher prevalence of comorbidities among cannabis users compared to non-users, may potential influence results and perceptions. Fourth, the survey only assessed the frequency and mode of administration and did not account for the dosage and precise composition of THC and CBD within the cannabis products being consumed. Fifth, the study was conducted in an academic, urban setting and limited to patients referred for Orthopaedic consultation, which limits the generalizability of these results to the broader MSK pain population. Finally, data collection started weeks following legalization at a single time interval, therefore the patient’s patterns and perceptions of cannabis efficacy and safety may change with increased awareness, social acceptability, and/or cannabis education since the time of the survey. We aim to repeat this work in the coming years to assess changes in use over time and collect validated patient reported outcome measures between cannabis users and non-users with chronic MSK pain, which will aim to improve upon some of the limitations identified herein.
Conclusion
One in five patients presenting to an orthopaedic surgeon with chronic MSK pain are using or have used cannabis with the specific intent to manage their pain, and most report it to be effective. Among non-users, two-thirds reported an interest in using cannabis to manage their MSK pain, but common barriers to use existed. Future double-blind placebo-controlled trials are required to understand if this reported efficacy is accurate, and what role, if any, cannabis may play in the management of chronic MSK pain.
Availability of data and materials
All data generated or analysed during this study are included in this published article [and its supplementary information files].
References
-
Ajrawat P, Yang Y, Wasilewski E, et al. Medical Cannabis Use and Inflammatory Cytokines and Chemokines Among Adult Chronic Pain Patients. Cannabis Cannabinoid Res. 2022. https://doi.org/10.1089/can.2022.0143.
-
Alsherbiny MA, Li CG. Medicinal Cannabis-Potential Drug Interactions. Medicines (Basel) 2018;6(1). https://doi.org/10.3390/medicines6010003.
-
Ashaye T, Hounsome N, Carnes D, et al. Opioid prescribing for chronic musculoskeletal pain in UK primary care: results from a cohort analysis of the COPERS trial. BMJ Open. 2018;8(6):e019491. https://doi.org/10.1136/bmjopen-2017-019491.
-
Benjamini Y, Hochberg Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. Journal of the Royal Statistical Society: Series B (Methodological). 1995;57(1):289–300. https://doi.org/10.1111/j.2517-6161.1995.tb02031.x.
-
Bhashyam AR, Young J, Qudsi RA, et al. Opioid Prescribing Patterns of Orthopedic Surgery Residents After Open Reduction Internal Fixation of Distal Radius Fractures. J Hand Surg Am. 2019;44(3):201-207 e2. https://doi.org/10.1016/j.jhsa.2018.11.003.
-
Bjordal JM, Ljunggren AE, Klovning A, et al. Non-steroidal anti-inflammatory drugs, including cyclo-oxygenase-2 inhibitors, in osteoarthritic knee pain: meta-analysis of randomised placebo controlled trials. BMJ. 2004;329(7478):1317. https://doi.org/10.1136/bmj.38273.626655.63.
-
Boehnke KF, Scott JR, Litinas E, et al. Pills to Pot: Observational Analyses of Cannabis Substitution Among Medical Cannabis Users With Chronic Pain. J Pain. 2019;20(7):830–41. https://doi.org/10.1016/j.jpain.2019.01.010.
-
Bot AG, Bekkers S, Arnstein PM, et al. Opioid use after fracture surgery correlates with pain intensity and satisfaction with pain relief. Clin Orthop Relat Res. 2014;472(8):2542–9. https://doi.org/10.1007/s11999-014-3660-4.
-
Bottorff JL, Bissell LJ, Balneaves LG, et al. Perceptions of cannabis as a stigmatized medicine: a qualitative descriptive study. Harm Reduct J. 2013;10:2. https://doi.org/10.1186/1477-7517-10-2.
-
Carney JJ, Hwang A, Heckmann N, et al. Characteristics of Marijuana Use Among Orthopedic Patients. Orthopedics. 2020;43(2):108–12. https://doi.org/10.3928/01477447-20191212-07.
-
Cohn AM, Johnson AL, Rose SW, et al. Support for Marijuana Legalization and Predictors of Intentions to Use Marijuana More Often in Response to Legalization Among U.S. Young Adults. Subst Use Misuse. 2017;52(2):203–13. https://doi.org/10.1080/10826084.2016.1223688.
-
Corroon J, Phillips JA. A Cross-Sectional Study of Cannabidiol Users. Cannabis Cannabinoid Res. 2018;3(1):152–61. https://doi.org/10.1089/can.2018.0006.
-
Craft S, Winstock A, Ferris J, et al. Characterising heterogeneity in the use of different cannabis products: latent class analysis with 55 000 people who use cannabis and associations with severity of cannabis dependence. Psychol Med. 2020;50(14):2364–73. https://doi.org/10.1017/S0033291719002460.
-
Dunn KM, Saunders KW, Rutter CM, et al. Opioid prescriptions for chronic pain and overdose: a cohort study. Ann Intern Med. 2010;152(2):85–92. https://doi.org/10.7326/0003-4819-152-2-201001190-00006.
-
Dunn SL, Wilkinson JM, Crawford A, et al. Expression of Cannabinoid Receptors in Human Osteoarthritic Cartilage: Implications for Future Therapies. Cannabis Cannabinoid Res. 2016;1(1):3–15. https://doi.org/10.1089/can.2015.0001.
-
Fitzcharles MA, Ste-Marie PA, Clauw DJ, et al. Rheumatologists lack confidence in their knowledge of cannabinoids pertaining to the management of rheumatic complaints. BMC Musculoskelet Disord. 2014;15:258. https://doi.org/10.1186/1471-2474-15-258.
-
Frane N, Stapleton E, Iturriaga C, et al. Cannabidiol as a treatment for arthritis and joint pain: an exploratory cross-sectional study. J Cannabis Res. 2022;4(1):47. https://doi.org/10.1186/s42238-022-00154-9.
-
Freeman TP, Lorenzetti V. “Standard THC units”: a proposal to standardize dose across all cannabis products and methods of administration. Addiction. 2020;115(7):1207–16. https://doi.org/10.1111/add.14842.
-
Greis A, Larsen E, Liu C, et al. Perceived Efficacy, Reduced Prescription Drug Use, and Minimal Side Effects of Cannabis in Patients with Chronic Orthopedic Pain. Cannabis Cannabinoid Res. 2022;7(6):865–75. https://doi.org/10.1089/can.2021.0088.
-
Haroutounian S, Ratz Y, Ginosar Y, et al. The Effect of Medicinal Cannabis on Pain and Quality-of-Life Outcomes in Chronic Pain: A Prospective Open-label Study. Clin J Pain. 2016;32(12):1036–43. https://doi.org/10.1097/AJP.0000000000000364.
-
Hathaway AD, Comeau NC, Erickson PG. Cannabis normalization and stigma: Contemporary practices of moral regulation. Criminology & Criminal Justice: An International Journal. 2011;11:451–69. https://doi.org/10.1177/1748895811415345.
-
Hazekamp A, Ware MA, Muller-Vahl KR, et al. The medicinal use of cannabis and cannabinoids–an international cross-sectional survey on administration forms. J Psychoactive Drugs. 2013;45(3):199–210. https://doi.org/10.1080/02791072.2013.805976.
-
Heng M, McTague MF, Lucas RC, et al. Patient Perceptions of the Use of Medical Marijuana in the Treatment of Pain After Musculoskeletal Trauma: A Survey of Patients at 2 Trauma Centers in Massachusetts. J Orthop Trauma. 2018;32(1):e25–30. https://doi.org/10.1097/BOT.0000000000001002.
-
Iffland K, Grotenhermen F. An Update on Safety and Side Effects of Cannabidiol: A Review of Clinical Data and Relevant Animal Studies. Cannabis Cannabinoid Res. 2017;2(1):139–54. https://doi.org/10.1089/can.2016.0034.
-
Kandel DB. Examining the Gateway Hypothesis: Stages and pathways of drug involvement. In: Stages and pathways of drug involvement: Examining the Gateway Hypothesis. Cambridge University Press: New York, NY, US; 2002; pp. 3-15.
-
Keyhani S, Steigerwald S, Ishida J, et al. Risks and Benefits of Marijuana Use: A National Survey of U.S. Adults. Ann Intern Med. 2018;169(5):282–90. https://doi.org/10.7326/M18-0810.
-
Koehler RM, Okoroafor UC, Cannada LK. A systematic review of opioid use after extremity trauma in orthopedic surgery. Injury. 2018;49(6):1003–7. https://doi.org/10.1016/j.injury.2018.04.003.
-
Kondrad E, Reid A. Colorado family physicians’ attitudes toward medical marijuana. J Am Board Fam Med. 2013;26(1):52–60. https://doi.org/10.3122/jabfm.2013.01.120089.
-
La Porta C, Bura SA, Negrete R, et al. Involvement of the endocannabinoid system in osteoarthritis pain. Eur J Neurosci. 2014;39(3):485–500. https://doi.org/10.1111/ejn.12468.
-
Langman MJ, Weil J, Wainwright P, et al. Risks of bleeding peptic ulcer associated with individual non-steroidal anti-inflammatory drugs. Lancet. 1994;343(8905):1075–8. https://doi.org/10.1016/s0140-6736(94)90185-6.
-
Liu CW, Bhatia A, Buzon-Tan A, et al. Weeding Out the Problem: The Impact of Preoperative Cannabinoid Use on Pain in the Perioperative Period. Anesth Analg. 2019;129(3):874–81. https://doi.org/10.1213/ANE.0000000000003963.
-
Lucas P, Walsh Z. Medical cannabis access, use, and substitution for prescription opioids and other substances: a survey of authorized medical cannabis patients. Int J Drug Policy. 2017;42:30–5. https://doi.org/10.1016/j.drugpo.2017.01.011.
-
Manchikanti L, Abdi S, Atluri S, et al. American Society of Interventional Pain Physicians (ASIPP) guidelines for responsible opioid prescribing in chronic non-cancer pain: Part I–evidence assessment. Pain Physician. 2012;15(3 Suppl):S1-65.
-
Medina SH, Nadarajah V, Jauregui JJ, et al. Orthopaedic surgery patients who use recreational marijuana have less pre-operative pain. Int Orthop. 2019;43(2):283–92. https://doi.org/10.1007/s00264-018-4101-x.
-
Meng H, Page MG, Ajrawat P, et al. Patient-reported outcomes in those consuming medical cannabis: a prospective longitudinal observational study in chronic pain patients. Can J Anaesth. 2021;68(5):633–44. https://doi.org/10.1007/s12630-020-01903-1.
-
Miller RJ, Miller RE. Is cannabis an effective treatment for joint pain? Clin Exp Rheumatol. 2017;35 Suppl 107(5):59–67.
-
Mucke M, Phillips T, Radbruch L, et al. Cannabis-based medicines for chronic neuropathic pain in adults. Cochrane Database Syst Rev. 2018;3(3):CD012182. https://doi.org/10.1002/14651858.CD012182.pub2.
-
Noble M, Treadwell JR, Tregear SJ, et al. Long-term opioid management for chronic noncancer pain. Cochrane Database Syst Rev. 2010;2010(1):CD006605. https://doi.org/10.1002/14651858.CD006605.pub2.
-
Pinto D, Song J, Lee J, et al. Association Between Sedentary Time and Quality of Life From the Osteoarthritis Initiative: Who Might Benefit Most From Treatment? Arch Phys Med Rehabil. 2017;98(12):2485–90. https://doi.org/10.1016/j.apmr.2017.06.004.
-
Piper BJ, Beals ML, Abess AT, et al. Chronic pain patients’ perspectives of medical cannabis. Pain. 2017;158(7):1373–9. https://doi.org/10.1097/j.pain.0000000000000899.
-
Power JD, Perruccio AV, Gandhi R, et al. Factors Associated With Opioid Use in Presurgical Knee, Hip, and Spine Osteoarthritis Patients. Arthritis Care Res (Hoboken). 2019;71(9):1178–85. https://doi.org/10.1002/acr.23831.
-
R RDCT. R: A Language and Environment for Statistical Computing. 2011. https://doi.org/10.1007/978-3-540-74686-7.
-
Renslo B, Greis A, Liu CS, et al. Medical Cannabis Use Reduces Opioid Prescriptions in Patients With Osteoarthritis. Cureus. 2022;14(1):e21564. https://doi.org/10.7759/cureus.21564.
-
Rotermann M, Page MM. Prevalence and correlates of non-medical only compared to self-defined medical and non-medical cannabis use, Canada, 2015. Health Rep. 2018;29(7):3–13.
-
Rudski JM. Treatment Acceptability, Stigma, and Legal Concerns of Medical Marijuana Are Affected by Method of Administration. J Drug Issues. 2014;44(3):308–20. https://doi.org/10.1177/0022042613511441.
-
Sampasa-Kanyinga H, Hamilton HA, LeBlanc AG, et al. Cannabis use among middle and high school students in Ontario: a school-based cross-sectional study. CMAJ Open. 2018;6(1):E50–6. https://doi.org/10.9778/cmajo.20170159.
-
Sandhu HS, Anderson LN, Busse JW. Characteristics of Canadians likely to try or increase cannabis use following legalization for nonmedical purposes: a cross-sectional study. CMAJ Open. 2019;7(2):E399–404. https://doi.org/10.9778/cmajo.20190008.
-
Satterlund TD, Lee JP, Moore RS. Stigma among California’s Medical Marijuana Patients. J Psychoactive Drugs. 2015;47(1):10–7. https://doi.org/10.1080/02791072.2014.991858.
-
Sims L, Goetz T, White N, et al. Cannabis use patterns among patients with upper extremity conditions at the time of legalization in Canada. Can J Surg. 2022;65(3):E335–41. https://doi.org/10.1503/cjs.004821.
-
Ste-Marie PA, Shir Y, Rampakakis E, et al. Survey of herbal cannabis (marijuana) use in rheumatology clinic attenders with a rheumatologist confirmed diagnosis. Pain. 2016;157(12):2792–7. https://doi.org/10.1097/j.pain.0000000000000706.
-
Sundstrup E, Jakobsen MD, Brandt M, et al. Regular use of pain medication due to musculoskeletal disorders in the general working population: Cross-sectional study among 10,000 workers. Am J Ind Med. 2016;59(11):934–41. https://doi.org/10.1002/ajim.22612.
-
Troutt WD, DiDonato MD. Medical Cannabis in Arizona: Patient Characteristics, Perceptions, and Impressions of Medical Cannabis Legalization. J Psychoactive Drugs. 2015;47(4):259–66. https://doi.org/10.1080/02791072.2015.1074766.
-
Vivace BJ, Sanders AN, Glassman SD, et al. Cannabinoids and orthopedic surgery: a systematic review of therapeutic studies. J Orthop Surg Res. 2021;16(1):57. https://doi.org/10.1186/s13018-021-02205-y.
-
Vyas MB, LeBaron VT, Gilson AM. The use of cannabis in response to the opioid crisis: A review of the literature. Nurs Outlook. 2018;66(1):56–65. https://doi.org/10.1016/j.outlook.2017.08.012.
-
Walsh Z, Callaway R, Belle-Isle L, et al. Cannabis for therapeutic purposes: patient characteristics, access, and reasons for use. Int J Drug Policy. 2013;24(6):511–6. https://doi.org/10.1016/j.drugpo.2013.08.010.
-
Ware MA, Doyle CR, Woods R, et al. Cannabis use for chronic non-cancer pain: results of a prospective survey. Pain. 2003;102(1–2):211–6. https://doi.org/10.1016/s0304-3959(02)00400-1.
-
Whiting PF, Wolff RF, Deshpande S, et al. Cannabinoids for Medical Use: A Systematic Review and Meta-analysis. JAMA. 2015;313(24):2456–73. https://doi.org/10.1001/jama.2015.6358.
-
Yelin E, Weinstein S, King T. The burden of musculoskeletal diseases in the United States. Semin Arthritis Rheum. 2016;46(3):259–60. https://doi.org/10.1016/j.semarthrit.2016.07.013.
Acknowledgements
Not applicable.
Funding
No funding was used for this study. Dr. Hance Clarke is supported in part by a Merit Award from the Department of Anaesthesiology and Pain Medicine at the University of Toronto.
Ethics declarations
Ethics approval and consent to participate
This study was approved by the UHN Research Ethics Board (REB Number: 18-5716).
Consent for publication
Not applicable.
Competing interests
Dr. Clarke is a principal investigator of an observational medical cannabis study funded by Shoppers Drug Mart. Dr. Clarke declares a previous relationship as a consultant to Scientus Pharma at the time of the grant. The consultant relationship ended in 2019 as such there are no conflicts with respect to this work and the opinions, results, and conclusions reported in this article are those of the authors and are independent of the funding sources. All other authors have no conflicts of interest or disclosures.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.